Moneshia Campus, Human Services Program Planner, emphasizes the importance of remembering the generational strength and perseverance of the Black community to promote healthier and happier lives.
What are diverse communities?
Diversity refers to the differences in backgrounds and cultures of people, including characteristics such as age, ethnicity, class, gender, disability, race, sexual orientation, income, education, gender identity, etc., as well as the overlapping – or intersectionality – of these attributes.
Strength of diverse communities
Diverse communities bring together people with different backgrounds, experiences, and viewpoints. This diversity of thought leads to more innovation, creativity, and a broader range of perspectives on everyday issues impacting people’s lives. When people of all backgrounds are treated with fairness and respect, it fosters a sense of belonging, reduces discrimination and prejudice, and allows people to build positive relationships, leading to stronger communities.
Challenges faced by diverse communities
Understanding the unique challenges and needs of diverse communities is essential to help determine how best to provide effective healthcare services, especially for substance use and mental health.
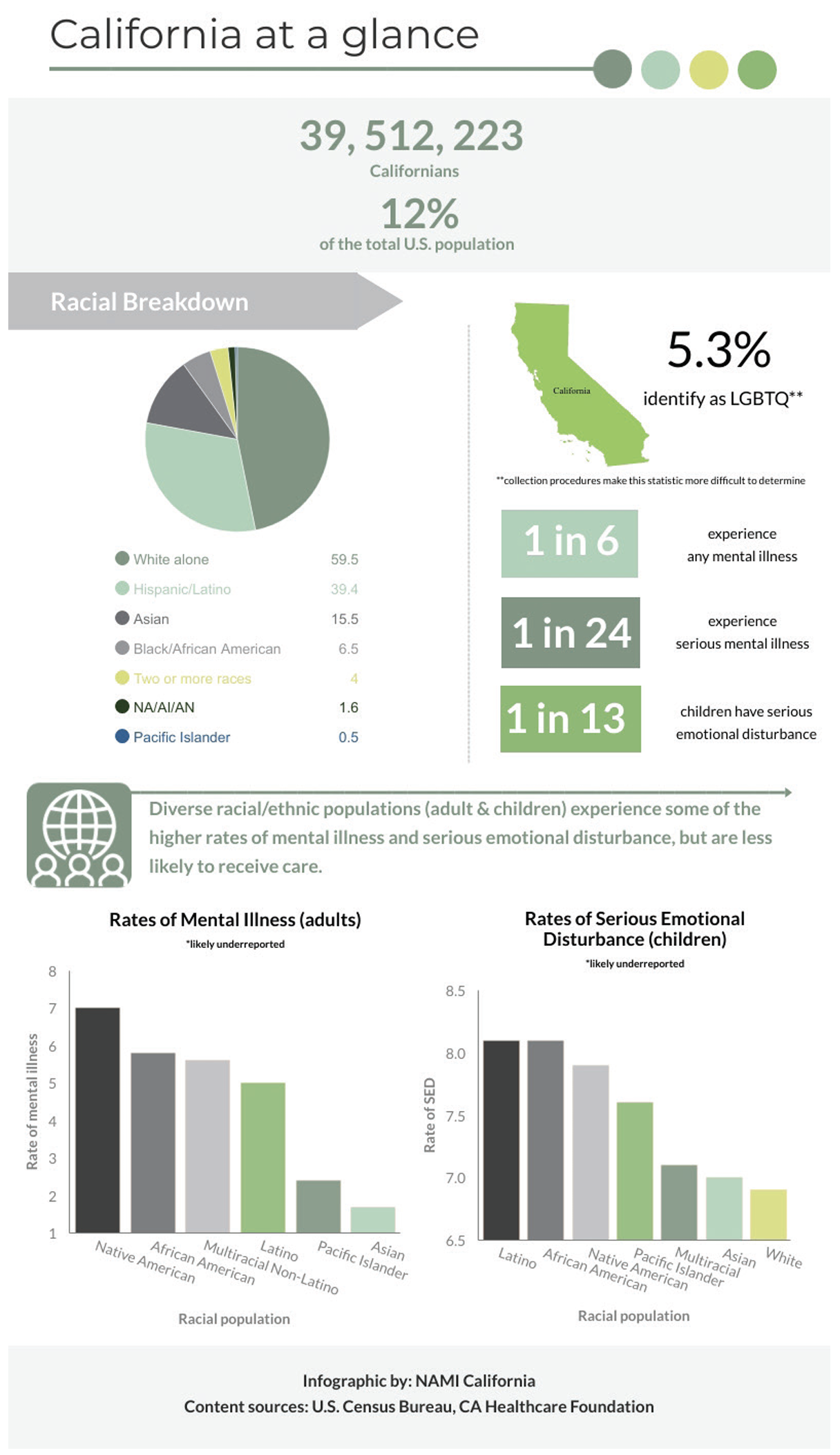
Sacramento County ranks 17th in the country in the 2020 Census Bureau's Diversity Index, which examines race and ethnicity. (1)
While Black/African American and Hispanic/Latino individuals make up 9.2% and 23.6% of SAC County’s demographic, respectively, they are overrepresented in the number of deaths county-wide.
Alarmingly, the fatal overdose rates for the Black, Latino/Hispanic, and Native American populations have risen sharply, nearly doubling for individuals in the Black and Hispanic communities. According to California Health Policy Strategies, Blacks/African Americans are the most overrepresented among overdose fatalities, especially Black women whose overdose deaths nearly tripled from 2015 to 2021. (2)
Likewise, as the National Alliance on Mental Illness (NAMI) reports, LGB adults have almost double the rate of substance use disorder (SUD) as compared to heterosexual adults, while transgender adults are nearly four times as likely to experience an SUD. The LGBTQ+ population experiences a higher rate of suicide, with high school students four times as likely to have attempted suicide. Transgender adults are especially overrepresented in suicide statistics, with 40% attempting suicide compared to less than 5% of the overall U.S. population. (3)
Causes of Disparities
Lack of cultural competence in the design and implementation of treatment and prevention programs. Culturally competent care addresses the experiences, background, and demographics of the individual. For example, research shows that, for historical reasons – mistreatment, racism, institutionalization, and deep-rooted stigma – individuals from Black communities can be resistant to mental health treatment. Very little research and resources have been dedicated to looking at culturally competent treatments for mental health or substance use. (4)
Structural barriers can impact access to quality healthcare. Access to quality healthcare varies widely among diverse communities. This is true for all aspects of healthcare, including substance use and mental health treatment. Socioeconomic factors, social policies, systemic barriers, community and neighborhood conditions, and healthcare inequalities contribute to the disparities in access to treatment facilities, support services, and culturally competent providers. People need to have access to facilities and providers in their own communities rather than in remote treatment locations that may be difficult to reach.
Socioeconomic factors can make treatment options less available. In 2018, 11.5% of Black adults in the U.S. had no health insurance. Communities of color are more likely to be hindered by a lack of resources – educational, health, and economic – that lead to reduced quality and access to care.
As a result of historical discriminatory policies, many Black Californians live in neighborhoods that are segregated and have high rates of poverty and unhealthy conditions. (5,6)
Cultural stigma and discrimination can deter people from seeking care. In many cultures, discussing mental health or substance use disorder and substance misuse is considered taboo, leading to a reluctance to seek help. This stigma can exacerbate the problem, discouraging individuals from accessing the support and treatment they need.
In NAMI’s State of the Community report for California, 60% of surveyed individuals in diverse communities, who sought mental health care, reported experiencing discrimination based on their race/ethnicity and/or cultural heritage, and over 40% experienced a lack of cultural awareness and racist language, attitudes, or beliefs. Similarly, while 40% of White individuals agreed that they felt comfortable talking with close family, friends, and community members about their mental health, the rates of those who agreed among minority communities were significantly lower. (7)
Often, individuals who use substances or have mental health disorders are characterized solely as criminals, dangerous, and a risk to communities. This further marginalizes people and serves as a barrier to getting them the needed help. Punitive policies disproportionally affect communities of color, with individuals in these communities more likely to be arrested for illegal drug use. For example, According to the National Institute of Health, Black people were more than four times more likely to be arrested for marijuana possession than White people in 2018, despite the two groups using the drug at similar rates. (8)
When you’re ready, we’re here for you.
Substance use and mental health
A 2022 national survey indicates that 48.7 million people aged 12 or older (or 17.3%) had a substance use disorder (SUD) in the past year. Substance use is a complex issue that affects individuals from all walks of life, transcending cultural, socioeconomic, and ethnic boundaries. However, the impact of substance use on diverse communities is often unique and requires a nuanced understanding. (9)
What many people don’t understand is that substance use disorders (SUDs) change the brain in many individuals, making drug use or misuse compulsive. When people are penalized for their addiction, it suggests a flaw in their character rather than a health condition that requires appropriate medical – and often behavioral – interventions.
According to SAMHSA, of individuals who need treatment for illicit substance use disorders, White individuals receive treatment 23.5% of the time, while Black and Hispanic individuals receive treatment 18.6% and 17.6% of the time.
Similarly, mental health conditions are not due to weakness or personal flaws. According to the 2022 SAMHSA survey, almost 1 in 4 adults aged 18 or older had a mental illness. Recognizing that mental health challenges are widespread, with over 20% of adults in the United States grappling with mental health conditions, is critical. These issues are not only treatable but often preventable. Rapidly changing demographics challenge mental health professionals to provide culturally relevant services that match the needs, values, and beliefs of a more culturally diverse society. (10)
Recognizing that substance use disorder and mental illness impacts all of us – friends, family, coworkers, neighbors – in some way is essential to shifting how we think about and treat those who are struggling.
When you’re ready, we’re here for you.
Addressing the challenges and needs of diverse communities
Promoting inclusivity and equity in mental health and substance use services
A report out of the University of Washington notes that most treatment programs for behavioral health disorders, including SUDs, have been developed and evaluated in predominantly White, heterosexual samples. (11) Efforts should be made to address the existing disparities by advocating for policies that promote equal access to affordable and culturally competent healthcare.
Foster inclusive communities that provide opportunities for underrepresented groups to have a voice and be represented in decision-making processes. This includes considering people’s intersectionality – how the overlapping, or intersection, of a person’s social identities related to age, disabilities, ethnicity, gender, geographic location, gender, socioeconomic status, sexuality, etc. – can impact in many ways.
The impact of substance use is often compounded by intersectionality, where individuals may face multiple forms of discrimination or disadvantage simultaneously. For example, LGBTQ+ individuals from minority communities may experience unique challenges that impact their substance use patterns and treatment outcomes.
Build culturally competent and responsive communities with the ability to understand, appreciate, and interact with people from cultures or belief systems different from one's own. Fostering cultural responsiveness means that the rich background of each individual is acknowledged, supported, and honored. These communities offer linguistically and culturally appropriate care informed by an individual and community’s values, norms, beliefs, experiences, intergenerational trauma, etc. This helps ensure that policies and practices are more reflective of the needs and concerns of all community members.
Explore cultural adaptation of existing evidence-based treatments for different groups. Cultural adaptive treatment looks at how traditional EBT (evidence-based treatment) can be modified to be more relevant and address a particular group's ideas, values, beliefs, norms, attitudes, and knowledge. Research suggests that adapting existing evidence-based treatments may lead to better outcomes in treatment. (12)
Community-defined evidence practices (CDEPs) that draw on the unique knowledge, experiences, and needs of local community residents in the development of programs, interventions, treatment protocols, and prevention strategies is one promising approach that is gaining traction. CDEPs test the approaches in clinical settings and then use the data gathered from historically marginalized community members to determine what is most effective.
Additional studies are needed to examine the impact of culturally competent treatments for diverse youth, as very little research exists. For sexual minorities, there is even less research that examines sexual orientation as a demographic variable. (11)
Reduce stigma and increase awareness in efforts to combat harmful stereotypes and encourage open dialogue about substance use and mental health. We must create opportunities and spaces in the community for individuals to openly share their experiences. Working to build trust and implement outreach through community-based programs, support groups, and educational initiatives that partner with local organizations and schools can improve outcomes.
Promote multifaceted empowerment at the community, family, and individual levels.
Empowering diverse communities to develop solutions is key to addressing the impact of substance use. Engaging everyone through community-based programs, support groups, and educational initiatives can play a pivotal role in fostering resilience and providing resources for prevention and treatment. Community-based initiatives and partnerships with local organizations can play a crucial role in bridging the gap and ensuring that everyone, regardless of their background, has access to the help they need. This approach also helps break down trust barriers and ensures that the support provided aligns with the unique needs of each community. Nurturing strong relationships helps improve public safety and health outcomes and creates stronger communities where every person can thrive.
References
(1) United States Census Bureau. (2021, August 12). Racial and Ethnic Diversity in the United States: 2010 Census and 2020 Census. Census.gov. https://www.census.gov/library/visualizations/interactive/racial-and-ethnic-diversity-in-the-united-states-2010-and-2020-census.html
(2) California Health Policy Strategies. (2023). Policy Brief Fatal Overdoses in California. https://calhps.com/wp-content/uploads/2023/04/2023-04_CalHPS_CA_Overdose_Report_Final.pdf
(3) National Alliance on Mental Illness. (2023). LGBTQI | NAMI: National Alliance on Mental Illness. www.nami.org. https://www.nami.org/Your-Journey/Identity-and-Cultural-Dimensions/LGBTQ
(4) Smith, K. (2020). Discrimination and Racism in the History of Mental Health Care | NAMI: National Alliance on Mental Illness. Nami.org. https://www.nami.org/Blogs/NAMI-Blog/July-2020/Discrimination-and-Racism-in-the-History-of-Mental-Health-Care
(5) National Alliance on Mental Illness. (n.d.). Mental health in Black communities: Challenges, resources, community voices. NAMI California. Retrieved February 23, 2024, from https://namica.org/mental-health-challenges-in-african-american-communities/#:~:text=mental%20health%20outcomes.
(6) Health, D. of P. (2023, October 4). Centering Black Mothers. Www.cdph.ca.gov. https://www.cdph.ca.gov/Programs/CFH/DMCAH/Pages/Health-Topics/Centering-Black-Mothers.aspx
(7) National Alliance on Mental Illness: California. (2020). Diverse communities: “Nothing about us without us.” National Alliance on Mental Illness, California. https://namica.org/wp-content/uploads/2021/06/ThirdRail-ASCYear3Report-Diverse-FINAL.pdf
(8) Abuse, N. I. on D. (2021, December 21). Stigma and Discrimination. National Institute on Drug Abuse. https://nida.nih.gov/research-topics/stigma-discrimination#references
(9) National Institute on Drug Abuse. (2023, November 13). HHS, SAMHSA Release 2022 National Survey on Drug Use and Health Data. Samhsa.gov. https://www.samhsa.gov/newsroom/press-announcements/20231113/hhs-samhsa-release-2022-nsduh-data#:~:text=In%202022%2C%2048.7%20million%20people
(10) Substance Abuse and Mental Health Services Administration, & U.S. Department of Health and Human Services. (2021). Racial/Ethnic Differences in Substance Use, Substance Use Disorders, and Substance Use Treatment Utilization among People Aged 12 or Older (2015-2019). SAMHSA.gov. https://www.samhsa.gov/data/sites/default/files/reports/rpt35326/2021NSDUHSUChartbook102221B.pdf
(11) Stoner, S. (2018). Effective Treatments for Substance Use Disorders in Racial, Ethnic, and Sexual Minorities: A Brief Review Effective Treatments for Substance Use Disorders in Racial, Ethnic, and Sexual Minorities: A Brief Review. https://adai.uw.edu/pubs/pdf/2018effectivetreatmentsforminorities.pdf
(12) Bernal, G., Jiménez-Chafey, M. I., & Domenech Rodríguez, M. M. (2009). Cultural adaptation of treatments: A resource for considering culture in evidence-based practice. Professional Psychology: Research and Practice, 40(4), 361–368. https://doi.org/10.1037/a0016401